
The downward spiral of pain and worry
I don’t know if it’s the sensation of pain that is the worst feeling, or if it’s losing the life that matters to you, but
It’s hard to feel safe and well once pain becomes a daily companion.
Most people that search for information about pain online read very scary and worrying information. Often that information is factually “correct”, because pain is usually a sign that there is something that is threatening your body.
Hence, what you read only points out the “red flags” that are medical problems that need attention. However, although these usually are not the cause of pain, this kind of information can cause you to worry even more that something serious might be wrong with your body.
Many people fear that they have cancer, because they read that back pain is a symptom of many forms of cancer on the internet. This is an understandable concern when you are in pain and are uncertain about its cause. However, back pain due to cancer is extremely rare.
Cancer is a worst case scenario. It does happen and it should not be missed in diagnosis, but the probability that your pain is caused by cancer is tiny.
Red flags rule out concerning causes of pain
In medicine, a “red flag” is a term that describes a sign or symptom that indicates an urgent or significant medical condition that needs rapid attention by a medical professional. Medicine excels at picking up these serious problems with scans and diagnostic tests. Red flags are the first layer of information that doctors check, to make sure you’re safe to relax and get moving again.
Ruling out red flags with a primary care doctor is a good way to decrease your fear of what is causing pain. This alone can help decrease your pain by reducing anxiety and tension, and also help you avoid unneeded emergency room visits and scans.
Some health care professionals describe an episode of pain as being a bit like a common cold. Most people will have it during their lives, and it recovers in a few weeks thanks to the natural history of recovery. Checking for red flags, or serious problems, is like making sure your common cold is not pneumonia or something more serious.
Red Flags: What you need to know
When we check for red flags, we’re looking out for the following diseases that need immediate attention and special care:
- cancer
- infection
- fractures
- abdominal aneurysm
- severe neurological compromise
These are the questions that we ask for red flag conditions.
1. Is your pain no better with rest?
2. Does your pain wake you at night?
3. Have you had cancer previously?
4. Have you lost of control of your bladder or bowels?
5. Do you have weakness or loss of feeling in your legs?
6. Do you have numbness between your legs (like you’ve been riding a horse)?
7. Are you over 50 years old?
8. Have you been taking corticosteroids?
“Yes” to any of these, along with other features of your pain, such as its location, severity, how long it has been present and if any particular event caused it, might raise your doctor’s suspicion that the cause of pain might be serious and should be investigated further.

Imaging and blood tests for Red Flags
If there is concern that your back pain and related symptoms might be due to any of the problems listed above, your doctor will likely order further testing to gather more information. Usually these tests are in the form of imaging studies and blood tests.
X-rays may not be good for visualizing
If you have a cancer history or suspicion that your pain is being generated by infection or injury to soft tissue, your doctor will probably send you for an MRI to get more detail.
The three most common cancers to metastasize or travel to the spine are:
- breast
- lung
- gastrointestinal (GI)
Many people find that medical scans, such as MRIs and x-rays, make them fearful when they don’t know what the words in the report mean.
You should know that a scan does not tell the entire story of what is happening in your body and in your life that could be contributing to your pain. In fact, it’s common for people to experience severe back pain, yet their scans don’t reveal anything that could be the source of their pain. Obviously, the pain people experience in these cases are still real.
This clearly demonstrates that scans are often unable to provide useful information about what is causing the pain, and should almost never be relied upon exclusively.
Just look at how many people have abnormalities with no pain:
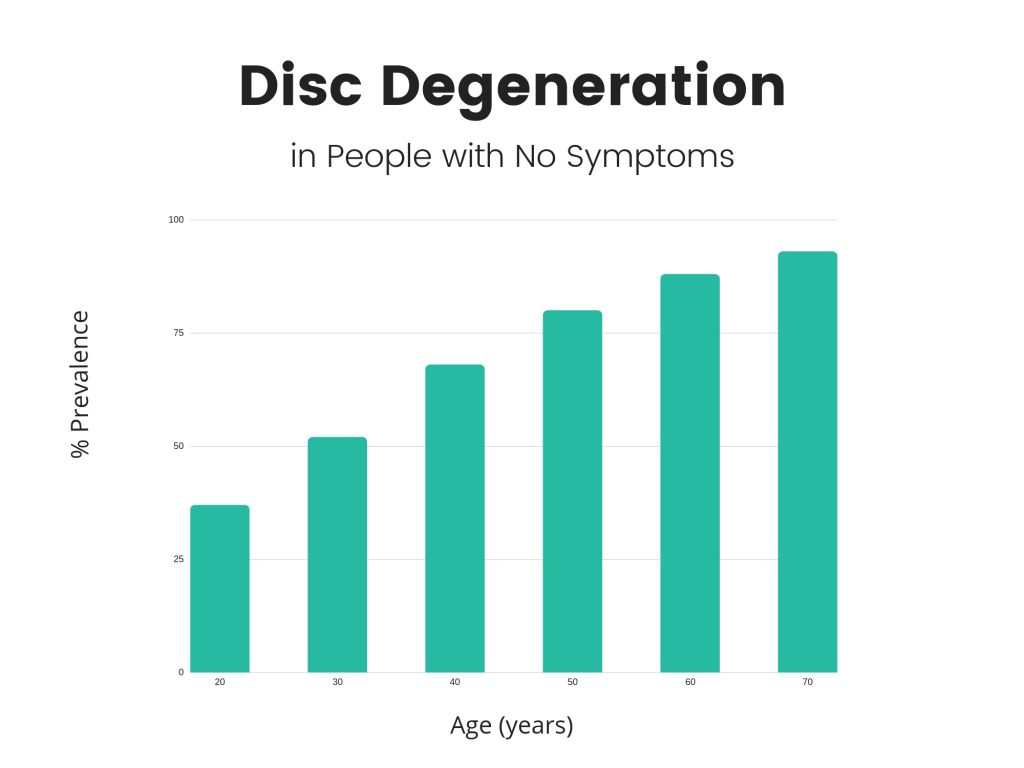
Imaging Features of Spinal Degeneration in Asymptomatic Populations,”
Am J Neuroradiol 2014 Nov 27: 1-6. [Epub ahead of print] 2014© by
American Society of Neuroradiology.
In addition to imaging, there are a variety of blood tests that can be used individually or collectively to help determine if your pain is a cause of concern.
For example:
- White blood cell counts can reveal information about infection and some cancers.
- Hemoglobin, hematocrit, and platelets can be affected by some cancers.
- Markers of inflammation, such as ESR and CRP can also point to the possibility of cancer or infection
- There are many new sensitive blood tests being developed for specific types of cancers
Other conditions associated with chronic back pain
Persisting pain is a feature of other medical conditions that involve a disease process affecting multiple systems of the body. This includes diseases like rheumatoid arthritis, ankylosing spondylitis, and lupus, all of which involve changes to the immune system and need to be medically managed with specialist care.
These conditions have specific treatments and medications used in their treatment and management. Your medical history, combined with imaging and blood tests, should reveal if you are affected by such diseases and direct you to the medical care you need.
Feeling safe when red flags are clear
The medical system is designed to find serious medical problems and treat them. Clearing the bad stuff is a relief, because you know you’re healthy overall, but what should you do if you’re still hurting?
There’s
PainChats exists to fill that gap, so we hope you can find some of the resources you need to get well here. It will definitely help to have a doctor who is knowledgable about the most up-to-date information about
Melissa Cady, D.O. is an American-trained osteopathic physician who is dual board-certified in anesthesiology and pain medicine. Melissa’s path has been unique with her history as a personal trainer, a physical therapy aide, and managing her own persistent pain. Known as the Challenge Doctor, Melissa wrote PAINDEMIC: A Practical and Holistic Look at Chronic Pain, the Medical System, and the antiPAIN Lifestyle, and created the Pain Out Loud website to help those in pain with more holistic and educational approaches to pain treatment.



 Treating Pain with Kindness 1: Getting Health Care that Helps
Treating Pain with Kindness 1: Getting Health Care that Helps
